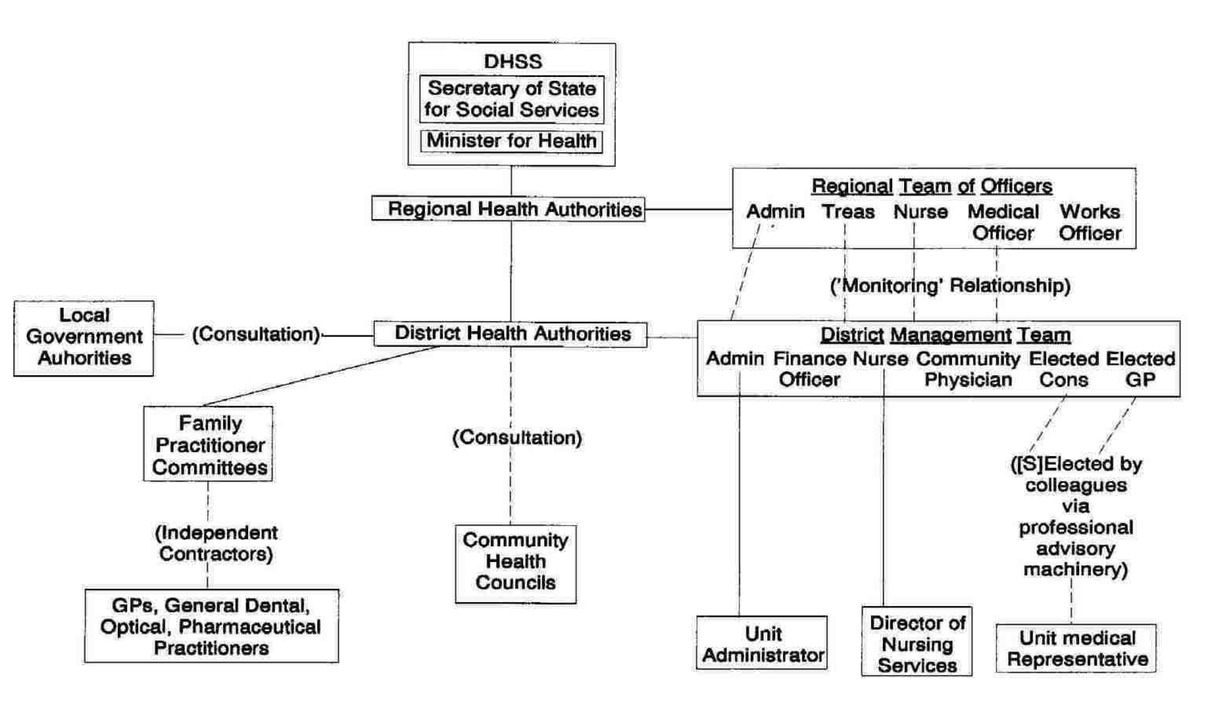
Outline organisational structure of English (and Welsh? - PB) NHS, 1982. From https://www.sochealth.co.uk/national-health-service/griffiths-report-october-1983/national-health-service-management-in-the-1980s/
A MANAGERIAL REVOLUTION
This apparently rather laid back 'consensus' system was challenged in 1983 by the 'Griffiths Report', commissioned by the Thatcher Government. The Griffiths Report is often presented as the beginnings of the process by which the NHS adopted a business model but it seems clear that the existing model was far from perfect and that in particular it was weak where a Socialist would want it to be strong - in planning. The chapters I am using from Harrison's book are available on the website of the Socialist Health Association yet he does not address the issue raised by Julian Tudor Hart - the problem of the 'inverse care law': 'The availability of good medical care tends to vary inversely with the need for it in the population served.' (In fairness it should be said that Harrison is mainly concerned with hospitals, Tudor Hart, here at least, with GP practises).
Tudor Hart was writing in 1971 after over twenty years of the NHS. He continues: 'the general conclusion must be that those most able to choose where they will work tend to go to middle class areas and that the areas with highest mortality and morbidity tend to get those doctors who are least able to choose where they will work ... Of 169 new general practitioners who entered practice in under-doctored areas between October 1968 and October 1969, 164 came from abroad ... The process of redistribution of GPs ceased by 1956 and by 1961 had gone into reverse; between 1961 and 1967 the proportion of people in England and Wales in under-doctored areas rose from 17% to 34%.'
These of course were not the terms in which the problem was understood by the Thatcher government. They were concerned mainly with the need to cut public expenditure. The freedom of doctors was a freedom to spend, with policy makers and administrators having little powers of resistance, or to evaluate or monitor the effectiveness of the profession. It was a system based on trust. In 1982, however, Norman Fowler, as Secretary of State for Social Services 'announced arrangements to "improve accountability" in the NHS. There were two elements to these arrangements: a review process and a set of performance indicators. The review process was intended to secure greater adherence to national policies and priorities than had previously been the case: "Each year Ministers will lead a Departmental review of the long-term plans, objectives and effectiveness of each Region with the Chairmen of the Regional Authorities and Chief Regional Officers. The aims of the new system will be to ensure that each Region is using the resources allocated to it in accordance with the Government’s policies – for example giving priority to services for the elderly, the handicapped and the mentally ill – and also to establish agreement … on the progress and development which the Regions will aim to achieve in the ensuing year ..."
'Unlike earlier attempts to use comparative data, the new indicators were ... to be compulsory.'
Later in the year he announced 'the experimental use of private firms of accountants to audit the accounts of heath authorities ...
'On 7 October 1982 it was announced that a firm of chartered accountants were to study the possibility of cash-limiting Family Practitioner Committee budgets [the Family Practitioner Committees administered the distribution of government funds to GPs in any given area - PB]. On 19 January 1983 central control of NHS manpower numbers was announced and on 4 February came the first public suggestion that the Government was seriously considering restrictions on doctors’ rights to prescribe; in November 1984 the withdrawal occurred from NHS prescriptions of a range of proprietary drugs which had been previously freely available. On 8 September 1983, health authorities were instructed to engage in competitive tendering for laundry, domestic, and catering services.'
This last has been widely blamed for a decline in the quality of these services, including 'the spread of "superbugs" being attributable to the cleaners no longer forming part of integrated care teams on wards.' (Jessica Ormerod: Legislation, Privatisation and the NHS, https://www.sochealth.co.uk/2018/06/13/34928/)